When every region on this planet has an adequate amount of mental health facilities, therapists, and medicine to treat its citizens, perhaps we can then say we’re entering a phase of global health success! Many people are living in war-torn areas, while others are dealing with natural disasters. These calamities take a toll on a person’s mental health. That is one reason why mental health experts are especially important for these global residents.
The References
The following resources have a wealth of information for individuals experiencing mental health conditions, for those providing emotional support to loved ones who’ve been diagnosed, and others without conditions who simply wish to become more knowledgeable regarding mental health sciences.
The Importance Of Relaxing
The following nature video (Relaxing Tree, 2020) is a reminder that visiting parks and listening to the sounds of nature can become a vital ingredient in having and maintaining calmness for positive mental health. It can become a method of getting away from it all periodically!
[VIDEO: 4K RELAXING NATURE SOUNDS – SHORT VIDEO CLIPS OF NATURE: SOURCE: RELAXING TREE, 2020]
Other forms of relaxation can involve meditating, engaging in yoga exercises, participating in arts such as sewing, crocheting, knitting, reading publications from favorite bookstores, and taking a walk after dinner, which can help reduce a few calories as an added benefit. Listening to quiet music, cooking/baking, gardening, housework, painting, sculpting, coloring in a coloring book, landscaping, drawing, building furniture, writing in a spiral notebook about one’s feelings and experiences, and watching television are also forms of relaxation.
A Person Should Never Label Oneself
An important aspect to remember is that just because a person is diagnosed with a mental health condition doesn’t suggest even remotely that they are a mental health condition. What the diagnosis means is that it’s another one of life’s challenges.
A Person Should Never Blame Themselves, Nor Compare Themselves
Some people will experience influenza and will suffer from symptoms temporarily. It could be because they’re younger, have no prior history of respiratory issues, and lack a compromised immune system. Conversely, other people may have a longer bout of the illness since they have a prior history of respiratory issues, they’re older, and already have a compromised immune system.
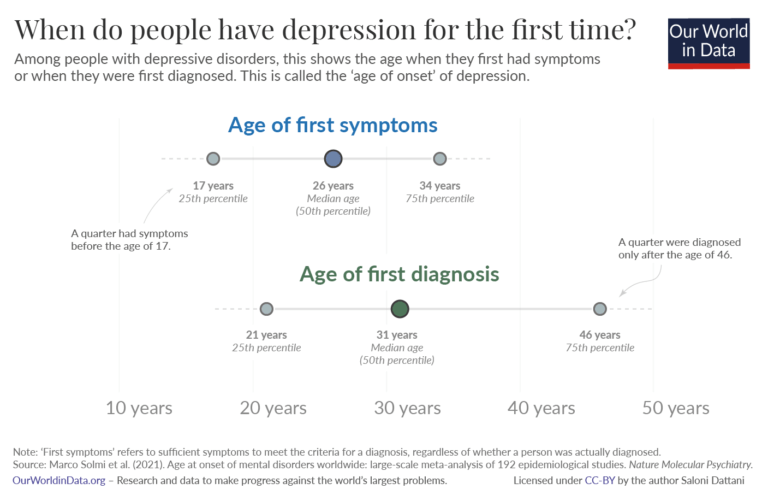
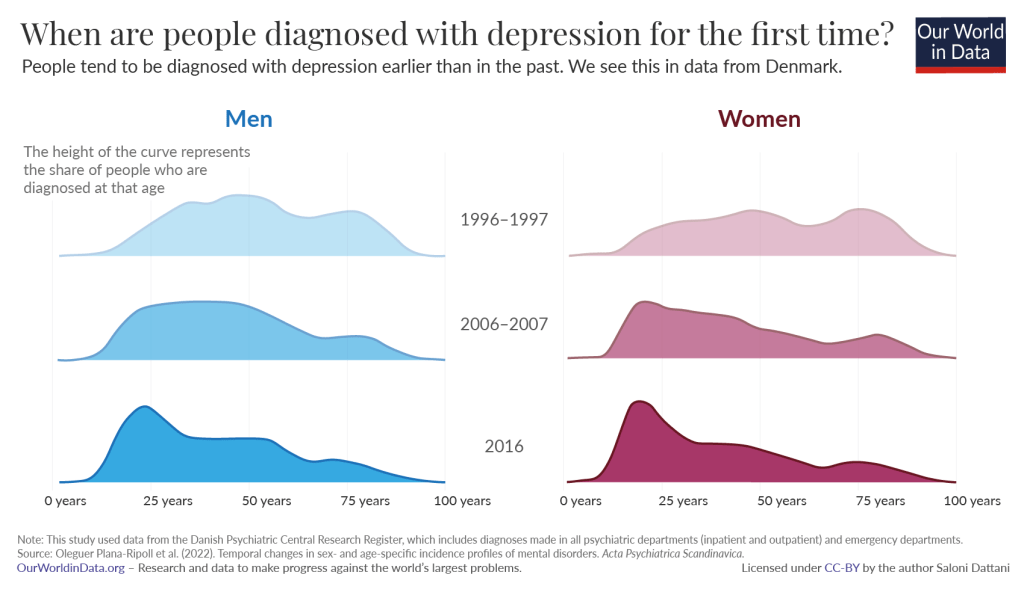
In a similar vein, each person who is diagnosed with a mental health condition may have a different reason for their mental health condition. For example, a person could be diagnosed with schizophrenia because they also have a form of Alzheimer’s Disease (i.e., comorbidity–more than one condition). Another person is diagnosed with schizophrenia because they have a sibling (twin) or a parent who was diagnosed with the condition years earlier (i.e., genetics). In taking the conversation in another direction, a person could be diagnosed with mild depression and needs medication temporarily because it began with becoming overwhelmed by life. They experienced too many negative personal life events. And then for another person diagnosed with depression, they may have to use prescriptions for the rest of their life because their brain chemistry has changed dramatically.
The associations, the causations, the bottom-up (i.e., physical illness bringing on the mental health condition), and other explanations are too involved and nuanced for the “How did this person acquire a mental health condition?” Thus, there can be any number of reasons why a person acquired a mental health difficulty, and it may not be a similar reason for other people with the same condition. Also, there could be situations where there are no known current explanations why someone ended up with a mental health condition, because those reasons are waiting for scientific discovery.
Getting Rid Of Stigmas
In the constant struggle to remove the stigma that remains in society concerning mental health challenges, people with psychiatric issues need to remember that they are not alone. Everyone has some form of mental health issue. Some mental health issues are minor, others are large, while others are dealing with comorbidity. Whatever the circumstance, everyone has something they’re dealing with. A person needs to keep going and live their life to the best of their ability!
There Is No Room For Negativity
Anyone who would make comments that a person with a mental health condition needs to “Get over it” or some other form of mocking/psychological abuse is not someone who should be in anyone’s social circle during the adjustment and recovery phase, and that could be for a lifetime. When a person is dealing with a psychiatric issue, they need supportive individuals who provide empathy and lots of encouragement. Actually, the toxic entities could be individuals who contributed to the mental health condition.
A Mental Health Issue Is Not Necessarily Psychiatric, Requiring Medication
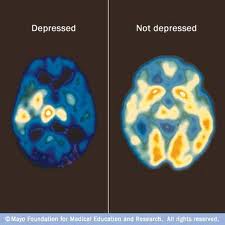
A psychiatric issue occurs when the brain chemistry has changed (i.e., an imbalance of a specific neurotransmitter) and a clinical therapist is required (i.e., psychiatrist). For instance, a person diagnosed with schizophrenia has an imbalance of dopamine (an imbalance of dopamine is associated with schizophrenia). Thus, medication is necessary to create a healthy brain chemistry. Other people may have phobias (i.e., height, insects, certain animals, specific places, etc.), and a psychologist would be suggested for learning techniques in removing said phobias. A psychologist is ideal when experiencing relationship difficulties. A psychologist might be used for cognitive behavioral therapy (CBT) to help a client learn new thinking strategies in maneuvering life, along with achieving goals.
The following is a video that talks about psychotherapy, which is a completely different brand of therapy altogether:
[VIDEO: WHAT IS PSYCHOTHERAPY? SOURCE: PSYCH HUB, 2020]
Family Members Becoming Involved In Their Loved Ones’ Journey
It cannot be emphasized enough that family members can make important contributions when a person is diagnosed with a psychiatric condition. Members can provide a guardrail of sorts in making certain that individuals keep doctor’s appointments with therapists and take prescribed medications. They can even attend these doctor appointments with their loved ones. The person diagnosed with a psychiatric condition can believe that they have partners in gaining a positive quality of life. In extreme cases, a family member may need to obtain conservatorship. All of these suggestions can avoid potential tragic situations with law enforcement, which we hear all too often in the media.
Weight Gain From Medications Is A Possibility, Although…
People who are diagnosed with a psychiatric condition need to ask the therapist for prescriptions that have a much lower possibility of weight gain. Many of these psychotropics and antidepressants (Bright Horizons Psychiatry, 2024) are not only responsible for a larger waistline, but also for the possibility of experiencing metabolic syndrome because of the additional weight gain (i.e., higher blood pressure, higher blood sugar leading to cardiovascular issues) (Cleveland Clinic, 2025). Conversely, a psychotropic and antidepressant may not necessarily cause actual weight gain. Taking these medications can result in a complete change to the body’s metabolism. Some individuals can experience fatigue, water retention, hormonal changes, and other modifications without additional calories to their diet (Bright Horizons Psychiatry, 2024).
As an aside, imagine the middle-aged woman who was already experiencing metabolic syndrome because of weight gain from hormonal changes (menopause), and is now prescribed an antidepressant or psychotropic. She will have to worry about even more weight gain difficulties, and unfortunately, could become a likely candidate for cardiovascular issues, and worse.
An Important No-No
If a person wants to go off their medication, that procedure needs to be done with the guidance of the therapist and gradually! Waking up one morning and deciding to cease taking medication can send an individual spiraling out of control, and with tragic consequences to themselves and others.
Finally, dealing with a mental health condition, especially one that has altered the brain chemistry, is rough! Having said that, once a person has gained clarity through doctor visits and taking medication, a person could use their condition and start anew with living their life instead of merely existing!
Here’s wishing you good health, love, and lots of understanding!
Vikki
References
American Academy Of Neurology. (2025). Brain Health For All. Retrieved From https://www.aan.com/
American Psychological Association. (2025). We promote psychological science and knowledge to benefit society and improve lives. Retrieved From apa.org
Behavioral Scientist. (2025). Health. Retrieved From https://behavioralscientist.org/topics/health/
Better Health Channel. (2022). Cognitive Behaviour Therapy (CBT). Retrieved From https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/cognitive-behaviour-therapy
Bright Horizons Psychiatry. (2024). Managing Weight Gain Caused By Psychiatric Medication. Retrieved From https://brighthorizonspsychiatry.com/managing-weight-gain-caused-by-psychiatric-medication/
Cleveland Clinic. (2025). Metabolic Syndrome. Retrieved From https://my.clevelandclinic.org/health/diseases/10783-metabolic-syndrome
deVries, L. P., van de Weijer, M. P., and Bartels, M. (2022). The Human Physiology Of Well-Being: A Systematic Review On The Association Between Neurotransmitters, Hormones, Inflammatory Markers, The Microbiome And Well-Being. (Vol. 139). https://doi.org/10.1016/j.neubiorev.2022.104733 Retrieved From https://www.sciencedirect.com/science/article/pii/S0149763422002226
Europe’s Journal Of Psychology. (2025). An Online-Only, Open-Access Journal For Scientific Inquiries Into A Wide Range Of Topics In Psychology – Free Of Charge For Authors And Readers. Retrieved From https://ejop.psychopen.eu/index.php/ejop
Healthcare Communications Network. (2025). Psychiatry. Retrieved From https://hcn.health/hcn-trends-story/category/psychiatry/
Healthline. (2025). Mental Well-Being. Retrieved From https://www.healthline.com/mental-health
JAMA Network. (2025). Psychiatry. Retrieved From https://jamanetwork.com/journals/jamapsychiatry
MDPI. (2025). Journal Of Behavioral Sciences. Retrieved From https://mdpi.com/journal/behavsci
MedicalNewsToday. (2025). Mental Health. Take Care Of Your Mental Well-Being With Evidenced-Backed Resources. Retrieved From https://www.medicalnewstoday.com/mental-health
Miller, C. (2025). Mental Health Disorders And Teen Substance Use. Why It’s Especially Tempting – And Risky – For Kids With Emotional Or Behavioral Challenges. Retrieved From https://childmind.org/article/mental-health-disorders-and-substance-use/
National Alliance On Mental Illness. (2025). Dissociative Disorders. Retrieved From https://www.nami.org/about-mental-illness/mental-health-conditions/dissociative-disorders/
Neuroscience News. (2025). Latest Neuroscience News. Retrieved From https://neurosciencenews.com/
NewScientist. (2025). Mind. Retrieved From https://www.newscientist.com/subject/mind/
Psyche. (2025). Know Your Self. Retrieved From https://psyche.co/
Psych Hub. (2020, November 3). What Is Psychotherapy? [VIDEO]. Retrieved From https://www.youtube.com/watch?v=wmHcB8aOlkI
Psychiatrist. (2025). Just Published. Retrieved From https://www.psychiatrist.com/
Relaxing Tree. (2020, October 10). 4K Relaxing Nature Sounds – Short Video Clips Of Nature. [VIDEO]. Retrieved From https://youtu.be/nqye02H_H6I?si=iHaQAgPVoU025-mF
ScienceDaily. (2025). Mind & Brain News. Retrieved From https://www.sciencedaily.com/news/mind_brain/
Smithsonian Magazine. (2025). Science/Mind & Body. Retrieved From smithsonianmag.com/category/mind-body
Taylor & Francis Online. The Journal Of Social Psychology. Latest Articles. Retrieved From https://www.tandfonline.com/action/showAxaArticles?journalCode=vsoc20
The British Psychological Society. (2025). Explore Psychological Publications. Retrieved From https://explore.bps.org.uk/
The Scientist. (2025). Exploring Life, Inspiring Innovation. Retrieved From https://www.the-scientist.com/tag/psychology
Therapy In A Nutshell. (2025). No One Ever Taught You How To Regulate Your Emotions. Let’s Change That Today. Retrieved From https://therapyinanutshell.com/
Thompson, D. (2025). Industrial Chemical Linked To Parkinson’s Disease. Retrieved From https://www.medicinenet.com/industrial_chemical_linked_to_parkinsons_disease/news.htm
Wiley Online Library. (2025) Psychiatry. Retrieved From https://onlinelibrary.wiley.com/action/doSearch?AllField=psychiatry
World Health Organization. (2025). Bipolar Disorder. Retrieved From https://www.who.int/news-room/fact-sheets/detail/bipolar-disorder
You must be logged in to post a comment.